What does the pancreas actually do?
The pancreas is a leaf shaped organ that makes up part of our digestive system.
Tucked underneath the liver, the pancreas is responsible for producing hormones like insulin and digestive juices that contain enzymes that break down food in the bowel.
About two hours after food is eaten, it flows down the pancreatic duct into the duodenum, which is joined to the stomach. When food reaches the duodenum, the exocrine pancreas releases its juices to help break down the food so it can be absorbed through the small bowel.
Meanwhile, in the endocrine pancreas, insulin is being produced and released directly into the bloodstream to convent glucose into energy, so that blood sugar levels remain stable.
How does pancreatic cancer affect the body?
The part of the pancreas that makes these digestive juices, the exocrine pancreas, is where pancreatic cancer occurs most frequently. In fact, it's estimated around 95% of pancreatic cancers are exocrine tumours, and the most common is PDAC, or pancreatic ductal adenocarcinoma.
In their early stages, pancreatic cancers don’t tend to exhibit many symptoms, or they’re easily missed because they come and go, but as the cancer grows and progresses, symptoms become much harder to ignore or miss. This often includes pain in the back or tummy, unintentional weight loss, appetite loss, indigestion, and changes in bowel habits.
Cancers can also develop in the endocrine pancreas, but they are much rarer. They behave differently, require different treatment, and cause different symptoms such as hormonal imbalances that affect insulin production. Named neuroendocrine tumours, this includes insulinoma, gastrinoma, glucagonoma, somatostatinoma and VIPoma.
How is pancreatic cancer typically managed or treated?
Treatments for pancreatic cancer vary depending on the location and stage of cancer, but surgery to remove the tumour and its surrounding cells is preferred when possible.
If pancreatic cancer is caught during stage 1 or 2, it's likely surgery will be scheduled. For some patients, chemotherapy may be recommended before surgery to shrink the cancer or slow its growth to increase the chance of surgery success, but chemotherapy is also routinely recommended after surgery to reduce the risk of the cancer coming back.
On occasion radiotherapy is also recommended either before or after surgery, but most patients will only ever receive one round of radiotherapy because it takes a quite brutal approach to cancer treatment, and in the case of pancreatic cancer often damages surrounding organs in the process.
If pancreatic cancer is discovered when it’s already reached stage 3 or 4, and it has become locally advanced cancer, unfortunately it's often inoperable, and care plans become focussed around chemotherapy or radiotherapy and symptom management.
And what about the symptoms associated with pancreatic cancer?
The main symptoms associated with pancreatic cancer tend to centre around digestion, from loss of appetite and unexpected weight loss, to bloating and bowel concerns like constipation. Pain in the back or abdomen are not uncommon, neither is jaundice, and vomiting and nausea regularly accompany chemotherapy treatment.
These symptoms are usually treated using a range of pharmaceutical medicines, from digestive aids, to painkillers and antiemetics. SSRIs or SNRIs are also frequently prescribed to help those affected manage the psychological effects of living with pancreatic cancer.
However, while these options work effectively for many - they aren’t always accessible. For example, CREON, a pancreatic enzyme replacement therapy, is commonly prescribed to patients with pancreatic cancer in the UK. But, at the moment there is a national shortage, and it's expected to last until 2026, So many are in search of CREON alternatives.
Can medical cannabis help with pancreatic cancer symptoms?
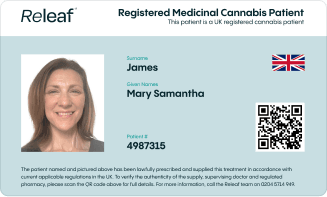
If the above therapies and treatments have proven to be unsuccessful at meeting your needs, or you’re unable to access them currently, you may be looking into alternative options - this is where medical cannabis might come in.
While in no way a cure or treatment for cancer itself, medical cannabis and cannabis-based products have shown promising potential in managing a number of the symptoms associated with pancreatic cancer, and these options have been legally accessible in the UK since 2018 through healthcare clinics like Releaf.
These products are generally very well tolerated and have a good safety profile when sourced from responsible, regulated producers like Glass Pharms. So, it's not surprising that many are now turning to this option for symptom support.
But, let’s be a bit more specific:
Can cannabis boost appetite for people with pancreatic cancer?
You may not be surprised to hear, medical cannabis - particularly THC - has shown to stimulate appetite, inducing hunger or ‘the munchies’.
For patients with pancreatic cancer this can be particularly useful, especially for those who have become disinterested in food, and can help to combat the unintentional weight loss that is so common for those affected.
While more research is needed in this area, studies also suggest that when applied appropriately, cannabis-based medicinal products may help to reduce inflammation and relax muscles in the digestive tract, in turn easing bowel movements and alleviating bloating.
Can medical cannabis help with cancer-related pain?
Medical cannabis has also shown promising results in managing cancer-related pain. Through its interaction with our endocannabinoid systems, medical cannabis can modulate - or influence - our perception or recognition of pain, which can be particularly beneficial for those with pancreatic cancer.
By reducing the perception of pain, the intensity is relieved, and this makes daily tasks much more manageable.
While cannabis-based medicines don’t eliminate pain, vast amounts of real-world evidence demonstrate their efficacy in this area, and now chronic pain is the most common condition treated with medical cannabis in the UK - and at Releaf.
Can I get medical cannabis for cancer-related depression or anxiety?
We know that battling with cancer often comes with mental health challenges such as depression and anxiety. If traditional approaches to treating and managing these secondary conditions haven’t been able to provide the support you need, you may be considered eligible for medical cannabis at Releaf.
This is because, when prescribed in the right concentrations and dosages, cannabis-based treatments have shown to relieve stress and aid relaxation. Strong real-world evidence also indicates they can have mood-uplifting effects and secondary benefits, such as improving sleep quality. Better sleep, in turn, supports emotional regulation.
Final thoughts from Expert Oncologist Dr Sue Clenton
Our Medical Director, Dr Sue Clenton has over 20 years of experience working as an Oncologist in the NHS. Throughout this time she supported thousands of patients throughout their journey with cancer, and this is something she continues to do today through Releaf, offering alternative solutions for those who’ve found conventional approaches ineffective.

We spoke to Dr Clenton to gain her insights on pancreatic cancer for this blog.
She told us:
“Cancer is never nice, but pancreatic cancer can be particularly nasty, and it brings some very debilitating and often overwhelming symptoms along with it. From the physiological impact of diagnosis, to the physical impact on appetite, to the side effects of conventional treatments: pancreatic cancer can really take its toll on a person.
I think that’s why I feel so passionate about ensuring that those affected are aware of all the options available to them, that they’re given accurate, and reliable information and the right support, so that they can make empowered, informed decisions about their treatment.
Alternative, more holistic treatments like medical cannabis aren’t right for everybody, but for some they can provide incredible relief and significantly improve quality of life - so it's definitely an option worth considering if conventional approaches aren’t meeting your needs, or are causing unpleasant side effects.”